INTRODUCTION
Recent studies have suggested that the prognosis of HIV-associated diffuse large B-cell lymphoma (HIV-DLBCL) may be improving with advances in anti-retroviral therapies (ART). A pooled analysis of clinical trial data showed that EPOCH may be associated with superior outcomes as compared to CHOP (Barta et al. Blood. 2013), but about two-third of patients in the combined analysis were treated without rituximab. A recent French study, however, showed similar overall survival (OS) between R-CHOP and R-EPOCH treated patients (Besson et al. AIDS 2017) and a phase III trial showed similar efficacy of R-CHOP vs. R-EPOCH in HIV-uninfected DLBCL (Bartlett et al. JCO 2019). The optimum frontline therapy in HIV-DLBCL is unknown as most clinical trials exclude HIV-infected patients or restrict accrual to those with undetectable HIV viral load and minimum CD4 count cut-off. Moreover, most existing studies include a majority (>60%) Caucasian population, and there is a paucity of studies on outcomes in African-American population. In this retrospective study, we describe the clinical features and outcomes of HIV-DLBCL patients seen at our institution and compare them with HIV negative DLBCL patients.
METHODS
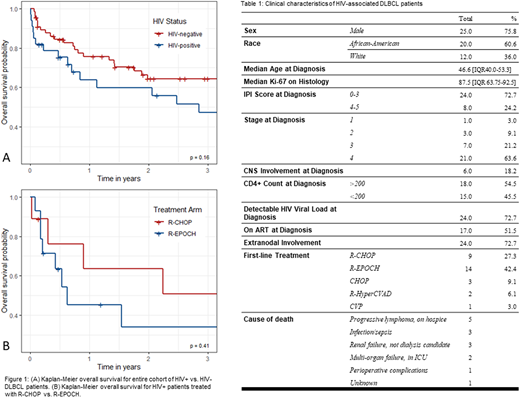
We conducted a retrospective review of HIV+ DLBCL cases diagnosed and treated at our institution from 2008-2020. We used the Kaplan-Meier method to assess overall survival (OS). Univariate and multivariate analyses were performed to assess prognostic factors. HIV-DLBCL patients were matched 1:2 with HIV negative DLBCL by age and stage of lymphoma at diagnosis. Comparison of OS analysis was conducted using log-rank method and predictors of progression or death using Cox proportional hazards regression.
RESULTS
We included a total of 33 patients with HIV-DLBCL in our study. Median age was 46.6 years (IQR 40-53.3), 25 (76%) were males, and 20 (61%) were African-Americans (Table). 28 (85%) patients had stage III/IV and 24 (73%) had extranodal disease at diagnosis. The median CD4 count at diagnosis was 252 (IQR 89.5-409). 6 (18%) had CNS involvement at diagnosis, for which the median OS was 8.3 months. First-line treatment included rituximab-chemotherapy combinations in 25 (76%) patients. All patients continued ART during first line treatment. Median follow up duration of the entire cohort was 2.06 years (IQR 0.53-5.02 years) and 5 (15.2%) were lost to follow up. The 2-year OS for R-CHOP treated patients was 63% vs. 38% for R-EPOCH treated patients, although this failed to reach statistical significance (p=0.125). On multivariate analysis, the only factor significantly associated with difference in event free survival (EFS; progression or death) was female sex (HR 19.86; [2.652-148.7]; p=0.004). Trends were seen towards shorter EFS among patients who were tobacco smokers at time of DLBCL diagnosis (HR 2.69; 0.463-15.6]; p=0.271), CD4+ count <200 at time of DLBCL diagnosis (HR 2.39; [0.519-11.0]; p=0.264), IPI score >3 (HR 2.98; [0.480-18.5]; p=0.241), and presence of MYC gene rearrangement (HR 3.93; [0.569-27.2]; p=0.165). Treatment type (R-CHOP, R-EPOCH), ART use prior to lymphoma diagnosis, race, and insurance status were not correlated with EFS. 11 (33.3%) patients died within 1 year of diagnosis. The 2-year OS for the entire cohort was 64% vs. 68% in matched HIV-negative DLBCL patients (p=0.651). Median OS for HIV+ patients was 2.14 years (IQR 0.23-5.77) vs 2.97 years (IQR 0.76-6.48) in matched HIV-negative DLBCL patients (p=0.3996). One patient died from acute hypoxemic respiratory failure prior to starting treatment. Four patients died of complications during their first inpatient chemotherapy administration.
CONCLUSION
In our cohort, most HIV-DLBCL patients were African-Americans, presented with advanced stage and extranodal disease. The survival of HIV-associated DLBCL was similar to HIV-negative counterparts. All HIV-DLBCL continued ART during chemotherapy, suggesting the feasibility of this approach. There was no difference in OS between patients treated with R-CHOP vs. R-EPOCH, however there was a trend towards increased OS in patients treated with R-CHOP. CNS involvement at diagnosis was frequently seen. Despite limited sample size, we observed a significant association with gender, and a trend toward significant factors including tobacco use and low CD4 count at time of diagnosis.
Mehta:TG Therapeutics:Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau;Merck:Research Funding;Roche-Genentech:Research Funding;Kite/Gilead:Research Funding;Innate Pharmaceuticals:Research Funding;Seattle Genetics:Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau;Oncotartis:Research Funding;Gelgene/BMS:Research Funding;Juno Parmaceuticals/BMS:Research Funding;fortyseven Inc/Gilead:Research Funding;Takeda:Research Funding;Incyte:Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau;Affimed:Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal